Social isolation, discrimination, and labeling are a part of the everyday struggles faced by the mentally ill. 1 in 4 American adults suffer from a mental illness. 1 in 17 people will have a serious mental illness such as schizophrenia, major depression and bipolar disorder. The stigma of mental illness ensures the majority of affected individuals will face negative consequences in recognizing and coping with their mental health needs.
 Erving Goffman defined mental illness as a blemish of character and a way to deviate from social norms. However, many of the definitions of mental illness fail to grasp that there are many other aspects to mental health. The three most influential social factors to mental illness are family stability, the placement of neighborhoods and society’s relationship to mental health problems. Mental illness does not solely arise from one’s environment. There are also biological and genetic predispositions that contribute to one’s mental health. One thing that is certain, as a society, we can change the way mental illness is perceived.
Erving Goffman defined mental illness as a blemish of character and a way to deviate from social norms. However, many of the definitions of mental illness fail to grasp that there are many other aspects to mental health. The three most influential social factors to mental illness are family stability, the placement of neighborhoods and society’s relationship to mental health problems. Mental illness does not solely arise from one’s environment. There are also biological and genetic predispositions that contribute to one’s mental health. One thing that is certain, as a society, we can change the way mental illness is perceived.
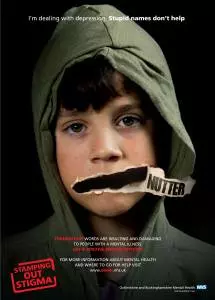
Social isolation or exclusion has been one of the most detrimental affects of the stigma, which is brought upon by labeling. The labels placed on the mentally ill by society, which the media reinforces, are dangerous, crazy, and inadequate. Due to these labels, those with mental illness get isolated from the rest of society. The practice of socialization then inevitably creates an “us vs. them” mentality, those people, the sane and the insane. Confided by these labels and exclusions, mental illness sufferers also struggle with finding their place in society.
Stand up against the stigma of mental illness is what society needs to create a new normal. This new normal will accept the importance of mental illness and will recognize treatment as equally important with physical illness. This new normal will place mental and physical health on the same spectrum. The new normal will make talking about mental illness a part of everyday conversation, and it will allow people to no longer be ashamed.
Hopefully with the acceptance of the new normal, it will bring about affordable mental health treatment, better counseling centers in high schools and colleges, and a society that is better educated on the issues of mental illness. With a new normal, those with mental illnesses can finally feel like they are a part of society and live without fear of isolation, discrimination, or labeling.
Listen to Episode 1 of my podcast Anxious Ramblings:
Anxious Ramblings is a biweekly conversation about mental illness. This show will challenge society’s views on the mentally ill and help to fight against the stigma. Anxious Ramblings explores the good, the bad, and the ugly side of living with a mental illness. Here we speak about all the crazy thoughts in your head that you’re afraid to say out loud.
For this episode of Anxious Ramblings, I introduce my story with Generalized Anxiety Disorder and speak about the stigma regarding mental illnesses. The episode concludes with me sharing responses from people who want to tell the world about their mental illness.
[audio