Approximately a week ago, I wrote an article asking Will Clinical Social Workers Embrace the New DSM 5 in light of the National Institute of Mental Health withdrawing its support for the publication. Then, Dr. Allen Francis wrote an article making a case for social workers not to embrace the DSM 5.
Responses by social workers on different social media outlets varied, but one unifying question remained….Why now? Historically, social workers have not been included in the developmental process of the DSM by the American Psychiatric Association (M.D.’s) despite being the largest provider of mental health services. I decided to email Dr. Frances and asked if he was available to answer some follow-up questions about his article on social workers.
He responded, “Sure…Let’s have a telephone call today. The week is very busy”. Dr. Frances spoke with me for almost a hour in order to help me relay the likely long term implications of the DSM V and why social workers being the largest stakeholders should be concerned too. This article is packed with resources because I independently verified every statement made by Dr. Frances in order for you to make your own assessment.
Before I dive into the interview with Dr. Frances, I would like to bring you up to speed with some background information on this not so new controversy.
What makes Dr. Allen Frances an authority on the DSM?
Dr. Allen Frances was chair for the DSM IV task force and the Department of Psychiatry at the Duke University School of Medicine, and he is currently a professor emeritus at Duke University. In late 2010, Dr. Frances did an in depth interview with Wired Magazine who had unlimited access to him as he reflected on almost two decades in the past when he authored the DSM IV. Here is an excerpt from Wired Magazine:
In its first official response to Frances, the APA diagnosed him with “pride of authorship” and pointed out that his royalty payments would end once the new edition was published—a fact that “should be considered when evaluating his critique and its timing.”
Frances, who claims he doesn’t care about the royalties (which amount, he says, to just 10 grand a year), also claims not to mind if the APA cites his faults. He just wishes they’d go after the right ones—the serious errors in the DSM-IV. “We made mistakes that had terrible consequences,” he says. Diagnoses of autism, attention-deficit hyperactivity disorder, and bipolar disorder skyrocketed, and Frances thinks his manual inadvertently facilitated these epidemics—and, in the bargain, fostered an increasing tendency to chalk up life’s difficulties to mental illness and then treat them with psychiatric drugs. Read Full Article
The article in Wired Magazine was indeed an eye opener. It discusses how an influential advocate for diagnosing children with bipolar disorder failed to disclose money received from the makers of the bipolar drug Resperdal. When viewed with a wider lens, it not really all that surprising considering the recent revelations on Attention Deficit Disorder as discussed in the New York Times.
History of Social Work Involvement with DSM
Back to the interview with Dr. Allen Frances, the first order of business was to gain some insight on the sudden outreach to the social work profession, and I didn’t anticipate learning something new. However, this was not the case.
Dr. Frances went on to tell me about Social Worker Janet B. Williams who was the text editor on the DSM III. Additionally, he also notes that she has been the only social worker ever to be included in the DSM development process. Currently, Janet Williams is the Vice President of Global Science at MedAvante. As stated in a 2011 PRNewswire Press Release, “MedAvante solutions help sponsors achieve enhanced assay sensitivity for increased drug effect and reduced trial failure rates, enabling them to bring better drugs to market faster.”
Dr. Frances acknowledged that social workers have not been represented in the development process despite being the largest provider of mental health services. However, he did state, “Social Workers have a huge stake in improving care for the really sick and should not be distracted by the expansions of the DSM V.”
DSM 5 Impact on Consumers
Dr. Frances expressed concerns for military service men and women being overly diagnosed with PTSD in lieu of allowing time for transitional services. Dr. Frances gives another example of how unemployment causes depression which is the result of environmental factors and not a mental illness.
Once someone regains employment and the situational stressors have abated, should this individual retain the label of a psychiatric disorder for seeking counseling as a coping mechanism? Do practitioners really want to label someone as a major depressive because they are unemployed or have been diagnosed with Cancer? Here is a video where Dr. Frances goes more in depth on the potential problems this will cause:
[youtube]http://www.youtube.com/watch?v=-AMvrcBvYWk[/youtube]
Unintended Consequences of DSM V
Dr. Frances stated one of the major issues with the DSM series is that its primary authors are research academics who are making suggestions and recommendations based on controlled research studies conducted in University clinics which are not helpful in everyday practice. By expanding the DSM 5 to cover challenges of everyday living, it will mislabel medical illness as a psychiatric disorder.
Dr. Frances also stated it will continue to foster an environment that diverts attention and resources away from the severely mentally ill and uninsured. As an example, Dr. Frances referenced the 1 million inmates in prison as a result of an undiagnosed and untreated mental health disorders due to poor resources and health care. Apparently, the Bureau of Justice Statistics agrees with him, and you can view their report here.
Dr. Frances quotes President Obama when he stated, “It’s easier to get a gun than an outpatient appointment.” Although gun control was not apart of our discussion, it should be noted that the National Rifle Association (NRA) is using its powerful lobbying efforts to change mental health thresholds and reporting laws in all 50 states.
Couple this type of legislation with over diagnosis by mental health professionals, the outcomes for children and families could be devastating. The New York Times does a great job of summarizing the presenting issues with current NRA proposals in an article entitled, The Focus on Mental Health Laws to Curb Violence is Unfair, Some Say. You can also view this video of Dr. Allen Frances speaking on the over diagnosis of mental illness:
[youtube]http://www.youtube.com/watch?v=yuCwVnzSjWA[/youtube]
Common Misconceptions About the DSM V
The interview with Dr. Allen Frances gave me an opportunity to ask him for clarification on some of the concerns expressed by social workers and their reasons for embracing the anticipated DSM 5. I made of a list of the main key points that he wanted Social Workers to know:
- The DSM is a copyrighted manual by the APA with no official authority with public or private health insurers.
- The ICD Codes are the only required codes necessary for billing mental health services. He states these codes are free of charge from the government with accompany resources and guides available. Here is the link found on CMS.Gov.
- The APA is motivated by earnings for publishing a new manual to cover budgetary shortfalls.
- Unless your institution demands use of the DSM V, Don’t buy it, don’t use it, and don’t teach it.
“The ICD is the global standard in diagnostic classification for health reporting and clinical applications for all medical diagnoses, including mental health and behavioral disorders. The United States will be one of the last industrialized countries to adopt the ICD-10, even though it was published in 1990.
Every member state of the World Health Assembly is expected to report morbidity and mortality statistics to the World Health Organization (WHO) using the ICD codes, but countries are allowed to modify the ICD for use within their own country.” ~Practice Central
Dr. Frances provided his twitter feed where he disseminates information on his current projects. He also stated to tweet your questions, comments, and concerns to @AllenFrancesMD as seen above.
Recommendations
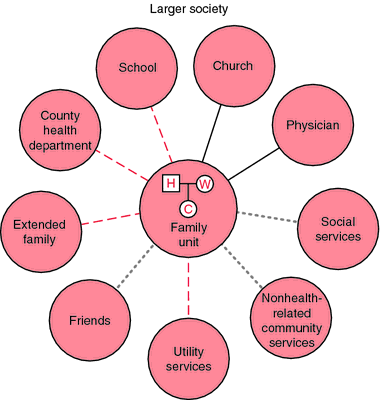
Dr. Frances states that he believes there should be a government arm similar to the FDA to help regulate, provide guidance for mental health providers, and make recommendations for public policy. He believes it should be comprised of an interdisciplinary team of psychiatry, social workers, and public health in order to create a holistic approach to treatment and diagnoses. Dr. Frances stated the APA should no longer have a monopoly on mental health especially with increasing influence from drug companies manifesting in their policies.
Also View:
Dr. Francis Op-ED in the New York Post
Don’t Buy it, Don’t Use it~Mother Jones
Find Him on Huffington Post